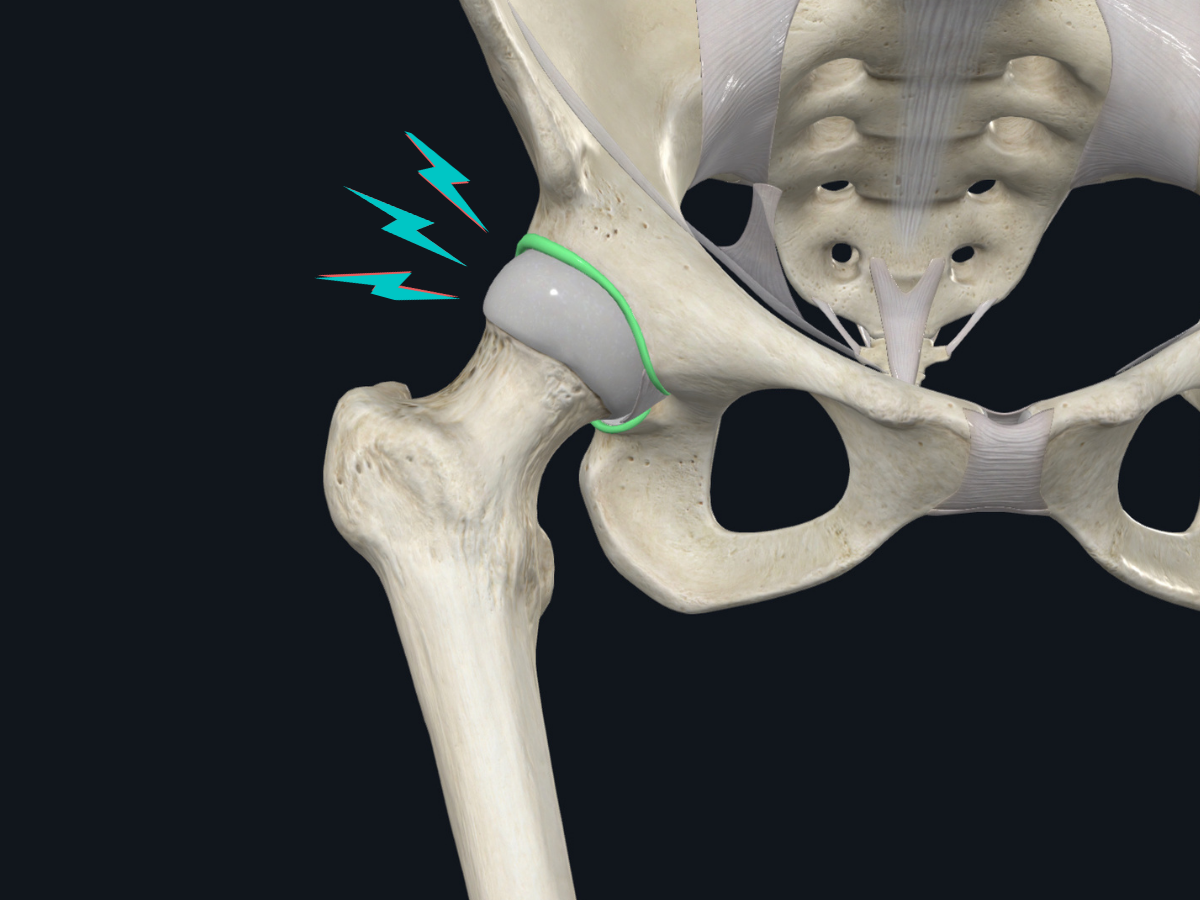
What is a labral tear?
A labral tear refers to damage to the labrum, a ring of cartilage that surrounds the hip socket (acetabulum). Think of the labrum as a gasket that deepens the hip socket and helps stabilize the ball-and-socket joint of your hip. When this cartilage is torn or damaged, it can cause pain and interfere with normal hip function.
The labrum serves several important functions:
- Deepens the hip socket to provide better stability
- Acts as a seal to help maintain joint fluid pressure
- Contains nerve endings that provide feedback about hip position
- Helps distribute forces across the hip joint
What causes labral tears?
Several factors can lead to labral tears:
Structural abnormalities:
- Cam lesions (extra bone growth on the femoral head)
- Pincer lesions (extra bone coverage of the hip socket)
- Hip dysplasia (shallow hip socket)
Activities and trauma:
- Sports involving repetitive hip flexion, adduction, and internal rotation
- Direct trauma to the hip
- Overuse or misuse of the hip joint
Other factors:
- Connective tissue disorders
- Age-related wear and tear
- Previous hip injuries
Athletes in sports like hockey, soccer, dance, and martial arts are at higher risk due to the repetitive motions these activities require.
What are the symptoms of a labral tear?
The most common symptoms that suggest a labral tear include:
Primary symptom cluster:
- Anterior (front) groin pain
- Pain that worsens with hip hyperflexion or sustained flexion positions
- Sharp, catching pain with rotational movements
Additional symptoms may include:
- Pain that worsens with sitting for long periods
- Clicking or catching sensations in the hip
- Stiffness in the hip joint
- Pain that radiates to the buttock or thigh
- Difficulty with activities like getting in and out of cars
The presentation is similar in both pediatric and adult patients, though the underlying causes may differ.
How are labral tears diagnosed?
Physical Examination
Your healthcare provider will perform several tests to assess for a labral tear:
Key physical examination tests include:
- FADIR (Flexion, Adduction, Internal Rotation) test
- FABER (Flexion, Abduction, External Rotation) test
- Range of motion assessment
Imaging Studies
Radiographs (X-rays):All patients with suspected labral tears should have X-rays taken, including:
- Standing anteroposterior (AP) pelvis view
- 45-degree Dunn view
These help identify underlying bone abnormalities that may have contributed to the labral tear.
Advanced Imaging: Magnetic Resonance Arthrography (MRA) is the preferred advanced imaging method for diagnosing labral tears. This involves injecting contrast dye into the hip joint before the MRI to better visualize the labrum.
Diagnostic Injection
If there's uncertainty about whether your pain is coming from inside the hip joint, your doctor may recommend a diagnostic hip injection. This involves injecting a local anesthetic (and sometimes a corticosteroid) directly into the hip joint. If your pain significantly improves after the injection, it suggests the problem is indeed within the joint.
How are labral tears classified?
Healthcare providers classify labral tears based on several factors:
- Pain level: Whether the tear causes pain or not
- Stability: Whether the torn piece is stable or unstable
- Repairability: Whether the tear can be surgically repaired
- Underlying bone structure: Associated cam/pincer lesions or dysplasia
- Joint condition: Presence or absence of arthritis
What are the treatment options?
Non-operative (Conservative) Management
Most patients should initially try non-operative treatment, which may be appropriate for:
- Minimal pain levels
- Chronic, long-standing tears
- Small tears
- Older or recreational athletes
- Absence of mechanical symptoms (catching, locking)
- No significant limitations in daily activities
Key components of conservative management include:
Multidisciplinary approach involving:
- Sports medicine physicians
- Physical therapists
- Athletic trainers
Treatment elements:
- Range of motion exercises
- Strengthening programs (especially core and gluteal muscles)
- Functional movement retraining
- Activity modification
- Patient education
- Symptom management techniques
Injections:Corticosteroid injections may help with symptoms, particularly if there's underlying degenerative change. The evidence for newer treatments like platelet-rich plasma (PRP) or viscosupplementation remains limited.
Return to sport-specific training:There's no specific timeline for returning to sport-specific activities during conservative treatment. The decision depends on:
- Strength levels
- Pain control
- Confidence and apprehension levels
- Sport-specific requirements
When is surgery considered?
Surgery may be recommended for patients with:
- Young or competitive athlete status
- Significant mechanical symptoms (catching, locking)
- Substantial limitations in daily activities
- Moderate to severe pain levels
- Failed conservative treatment (typically after several months)
Factors that affect surgical success:
- Patient age (younger patients typically do better)
- Pain severity
- Mental health status
- Overall health and absence of other medical conditions
- Obesity levels
- Previous rehabilitation attempts
- Duration of symptoms
- Type of underlying bone abnormality (cam vs. pincer lesions)
- Degree of joint degeneration
- Patient motivation
- Workers' compensation status
Surgical Options
Arthroscopic surgery is the preferred approach over open surgery for labral repair, reconstruction, or debridement, often combined with correction of underlying bone abnormalities (osteochondroplasty).
Potential surgical complications include:
- No improvement or worsening of symptoms
- Ongoing pain
- Risk of re-injury
- Loss of range of motion
- Blood clots
- Infection
- Nerve damage
- Heterotopic ossification (abnormal bone formation)
What about recovery and rehabilitation for hip labrum tears?
Post-operative Guidelines
Activity restrictions:There's ongoing debate about post-operative restrictions. Some considerations include:
- Range of motion restrictions may be based on the extent of surgery performed
- Weightbearing restrictions (some recommend partial weightbearing for 2 weeks)
- Hip abduction bracing is not routinely recommended
Rehabilitation timeline:
- Week 1: Isometric strengthening may begin
- 4-6 weeks: Eccentric and concentric strengthening programs
- 3 months minimum: Before return to sport for labral debridement
- 4-6 months minimum: Before return to sport for labral repairs
Return to Sport Criteria
Before returning to sports, patients should demonstrate:
- Pain-free activities
- Full range of motion
- Greater than 90% strength compared to the uninjured side (flexion, abduction, adduction, core)
- Sport-specific endurance
- Psychological readiness
- Good balance and proprioception
Sport-specific considerations:
- Cutting sports and deep flexion sports typically require longer recovery times
- Bilateral procedures may extend return-to-sport timelines
- Sports psychology evaluation should be included when available
When to seek revision surgery
If symptoms persist after initial surgery, revision surgery might be considered if:
- More than 12 months have passed since the initial surgery
- Imaging confirms ongoing pathology
- Appropriate post-operative rehabilitation has been completed
- There's evidence of incomplete bone correction
- Hip instability requires capsular reconstruction
- Diagnostic injection provides significant pain relief
What's the outlook?
The prognosis for labral tears varies significantly based on multiple factors:
Positive prognostic factors:
- Younger age
- Lower initial pain levels
- Good mental health
- Absence of significant arthritis
- Successful completion of rehabilitation
- High motivation levels
Challenging factors:
- Advanced age (particularly over 55)
- Severe degenerative changes
- Multiple medical conditions
- Poor compliance with therapy
- Workers' compensation cases
- Significant dysplasia
Most patients can expect significant improvement with appropriate treatment, though the timeline and degree of improvement vary considerably.
Important considerations
Timing matters: Early diagnosis and appropriate treatment can prevent progression of symptoms and joint damage. Delays in treatment may lead to:
- Increasing labral tear size and complexity
- Progressive cartilage damage
- Delayed return to function
- Worsening deconditioning
- Mental health impacts
Mental health: Your psychological well-being plays a crucial role in both recovery and outcomes. Don't hesitate to address anxiety, depression, or concerns about your condition with your healthcare team.
Second opinions: Given the complexity of these injuries, seeking a second opinion from a specialist experienced in hip preservation surgery can be valuable, particularly when surgery is being considered.
When to see a healthcare provider
You should consult a healthcare provider if you experience:
- Persistent groin or hip pain, especially with activity
- Catching or clicking sensations in the hip
- Pain that interferes with daily activities
- Symptoms that don't improve with rest and basic measures
Questions to ask your healthcare provider
- What specific type of labral tear do I have?
- What underlying bone abnormalities contribute to my condition?
- Am I a good candidate for conservative treatment?
- What are the realistic expectations for improvement with non-operative treatment?
- If surgery is recommended, what specific procedure would be performed?
- What are my individual risk factors for surgical complications?
- What would my rehabilitation timeline look like?
- When could I realistically return to my sport or activities?
Remember, every patient's situation is unique. This information should complement, not replace, discussions with your healthcare provider who can provide personalized recommendations based on your specific circumstances, activity goals, and medical history.


.png)

